Introduction
|
Product identification |
Version |
Release date |
|---|---|---|
|
AION |
v3.17.0.5 |
15/01/2026 |

| Basic UDI | UDI-DI | UDI-PI |
| PP 11956 AION 62 | 13 11956 AION-V.3 0 47 | v.3.17.0.5-2025-01-15 |
AION can be accessed via Nostos Genomics Variant Interpretation Platform ![]()
The use of the device is subject to the term and conditions provided on the log-in screen, and to the ITA (Individual Tier Agreement).
ℹ️ If you want to request a demo, or have any doubts or questions, please get in touch with Nostos Genomics through:
-
Our website: nostos-genomics.com
-
Our email: support@nostos-genomics.com
| Manufacturer | Nostos Genomics GmbH |
| Address |
c/o Stresemannstrasse 123 Tenant GmbH Stresemannstrasse 123 10963 Berlin Germany |
| Website | nostos-genomics.com |
|
Assignment of the products to the registration numbers in the German Medical Devices Information and Database System |
Nostos Genomics GmbH is a CDS (clinical decision support) software manufacturer registered with ID DE/0000049631 and included at IFA Liste under ID 117315, and CA Registration ID: DE/CA73/238029-01. SRN DE-MF-000035385 |
| Device ID | AION | |
| Basic UDI (BUDI) |
PP 11956 AION 62 |
|
| IVD/MD |
IVD SaMD Clinical Decision Support (CDS) |
|
|
IVDR Class & Conformance Route |
Rule 3-Class C-Genetic testing Annex IX-QMS Assurance |
|
|
Notified Body Name & ID# |
BSI the Netherlands Say Building, John M. Keynesplein 9, 1066 EP Amsterdam, Netherlands Certification Body ID#: 2797 |
|
|
BfArM-Registration numbers |
ID DE/0000049631 IFA Liste ID 117315 CA Registration ID: DE/CA73/238029-01 |
|
|
AION access (website) |
||
|
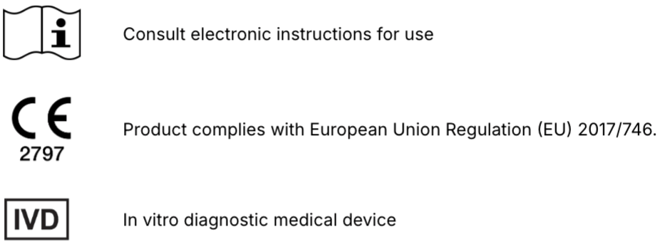
Product labelling |
|
|
Intended Use
AION is an in vitro diagnostic medical device software intended to qualitatively process next generation sequencing (NGS) data from genetic testing. This AI-driven IVD software identifies genetic variants, predicts their classification based on the integration of multiple annotation sources and generates a variant ranking based on disease association. AION is a semi-automated clinical-decision support software to assist healthcare professionals in making informed medical decisions regarding clinically relevant genetic variants and genetic diseases.
Indications for use
AION’s indication of use relates to mendelian genetic diseases testing. Genetic testing involves the detection and assessment of specific alleles, variants and genotypes, that are associated with heritable traits and diseases or predispositions to disease for the individual or their descendants (diagnostic, screening and predictive testing).AION’s Intended patient population includes patients of all ages (prenatal, postnatal), sex, and ancestries who might undergo NGS sequencing analysis with the aim of testing for genetic diseases.
Intended users
AION is intended to be used as part of the diagnostic workflow for NGS-based genetic testing by healthcare professionals (eg. human genetics professionals, geneticists, variant scientists, and healthcare practitioners with expertise in genetics). The software is not intended to be used by lay users.
Operating Principle
The AION software is a cloud-based clinical decision support (CDS) tool designed to facilitate the interpretation of genetic variants in the context of genetic diseases. Its primary function is to predict the pathogenicity of genetic variants using artificial intelligence (AI) models, leveraging the interpretation of next-generation sequencing (NGS) data.
- Input Data and Preprocessing:
- The software accepts VCF (Variant Call Format) files containing genetic variant information (small variants (SNVs, SNPs, INDELS) and CNVs/SVs) generated from secondary bioinformatic analysis of NGS data, including Whole Exome Sequencing (WES) and Whole Genome Sequencing (WGS). The VCF format recommendations are standardized across short-read sequencing platforms, predominantly Illumina (for further information see the IFU sections: VCF Format; Variant type, genomic regions and sequencing technologies; Limitations and Contraindications).
- Singletons (proband) and trios (proband-mother-father) are supported for small variants (for CNVs currently only probands are supported). In line with previous reports, trio analysis improves the variant classification performance over proband analysis. In addition, current analysis supports both reference genomes GRCh37/hg19 and GRCh38/hg38 which both performed with high quality. See information about AION VCF format, and variant types at Instructions for Use.
- For optimal variant prioritizer performance (variant ranking), the input may include patient clinical data, such as phenotypic features described using Human Phenotype Ontology (HPO) terms. Inclusion of HPO information is recommended (see section of Performance Characteristics) as it improves the variant ranking performance for both small variants (in singleton cases) and CNVs, where the effect is even more significant.
ℹ️ Including HPO terms is crucial for improving variant ranking performance, particularly in small variants (singleton cases) and CNVs. For CNVs, the inclusion of HPO data is especially important, as it significantly enhances ranking performance. We strongly recommend users provide HPO terms when analyzing CNVs to achieve optimal results.
- Upon submission, the software performs quality control checks on the VCF files to ensure data integrity. See recommendations about VCF format and quality criteria at the Instructions for Use section (VCF Format), following best practices for secondary analysis, and dependent on the NGS sequencing platform.
AION uses a comprehensive variant annotation pipeline that enriches the raw genetic data with relevant contextual information. This includes:
- Genetic Properties: Annotations such as evolutionary conservation scores (phyloP, phastCons) provide insight into the evolutionary importance of the genomic regions where variants occur.
- Molecular Properties: Predicted molecular consequences of the variants, such as whether they result in missense or frameshift mutations.
- Clinical Properties: Associations between variants and known genetic diseases, as well as related clinical phenotypes (HPO terms).
The complete list of annotations is as follows:
- Genomic position of the variant (chr, position, ref, alt)
- Characteristics of the variant in sequencing data (GT, GQ, DP, AD, VAF)
- Zygosity and segregation of the variant in the submitted samples(zygosity proband, zygosity mother, zygosity father, segregation)
- Reference gene, transcript and protein for annotations (hgnc_gene, hgnc_id, ENST_id, RefSeq_TranscriptID, exon_intron, HGVSc, ENSP_id, RefSeq_PeptideID, HGVSp)
- Predicted consequences of the mutation (most_sev_conseq, all_mut_types, impact)
- Population variant frequency (gnomAD_AC, gnomAD_AN, gnomAD_AF, gnomAD_hom, gnomAD_AC_genomes, gnomAD_AN_genomes, gnomAD_AF_genomes, gnomAD_hom_genomes, gnomAD_AC_exomes, gnomAD_AN_exomes, gnomAD_AF_exomes, gnomAD_hom_exomes)
- Evolutionary prediction scores (pCons46_ver, phyloP_ver)
- Splicing predictions (splice_type, dbscSNV_ada_score, dbscSNV_rf_score, NMD, NMD_boundary)
- Protein predictions (SIFT_class, SIFT_score, PolyPhen_class, PolyPhen_score, uniprot_domains)
- Gene haploinsufficiency scores (pLI, pRec, pNull, LOEUF, haploinsufficiency)
Variant classification is provided following three approaches:
- Public Database Annotations: The software incorporates classifications from public repositories like ClinVar (ClinVar classification, ClinVar_star_review, ClinVarID), which include expert-reviewed data on variant pathogenicity.
- Automated ACMG Classification: AION applies the American College of Medical Genetics and Genomics (ACMG) guidelines using a rule-based algorithm (ACMG_classification, ACMG_applied_rules ). This involves scoring each variant according to 28 criteria and assigning a classification based on these scores: “pathogenic”, “likely pathogenic”,"VUS” (Variant of Unknown Significance), likely benign" and "benign".This is currently the golden standard for variant classification.
- Proprietary AI Model - AION Predictor (see AI/ML Module within the AION Analytical Algorithm): AION employs a machine learning model trained to predict variant pathogenicity. This model considers various features, such as the functional impact on RNA and protein levels and constraints to variation (indicating the biological significance of the variant's location). The AION predictor (AION_classification, AION_variant_score) generates a classification and a confidence score for each variant, which are pre-computed and stored in a database. Based on this score, the algorithm provides a predicted variant classification: “pathogenic”(85% - 100%),“likely pathogenic” (60% - 85%),"VUS” (Variant of Unknown Significance, 40% - 60%), “likely benign" (15% - 40%) and "benign” (0% - 15%).
- The software outputs a ranked list of variants, prioritizing those most likely to be pathogenic based on a combination of annotation data, ACMG criteria, and AI-based predictions.
- Each variant is accompanied by a confidence score and detailed annotations, which include molecular effects, conservation data, population frequency, etc. This information aids genetic professionals in critically assessing the results.
- The list also includes potential gene-disease associations, with each variant linked to possible clinical diagnoses based on observed patient symptoms and known gene-disease relationships.
- AION offers both fully automated and semi-automated manual modes. In the semi-automated manual mode, users can apply custom filters to the annotated and classified variants, allowing for a more tailored analysis based on specific clinical questions or research interests.
- The software also supports variant storage and interpretation reporting, enabling ongoing case management and historical data analysis.
This comprehensive approach integrates bioinformatic data processing, AI-driven predictive modeling, and detailed annotation to assist healthcare professionals in making informed clinical decisions regarding genetic diseases.
⚠️ AION is a clinical-decision support IVD SW, as such no medically-relevant decisions should be made without first consulting the appropriate healthcare professional and/or information on disease effects, prevalence or others.
AION incorporates an Artificial Intelligence (AI) model to support the interpretation of diagnostic data. The AI analyses the input genetic data and provides suggested results based on patterns identified during its training. While the AI has been validated on clinically relevant data, its outputs may occasionally differ from expected findings. The AI is designed to assist and support the user, not to replace professional judgment. All AI-generated results must be reviewed and verified by the responsible healthcare professional before being used for clinical decision-making.
The AI model has been trained and validated on data relevant to the intended use. It is not intended to detect conditions outside this scope. To ensure safe and effective use, healthcare professionals should:
- Confirm AI-suggested results against their own clinical expertise and the available patient data.
- Report any unexpected or inconsistent outputs through the established feedback and customer support channels.
This ensures that the AI functions as a reliable decision-support tool while safeguarding the accuracy and integrity of the diagnostic process.
The AI model may be updated periodically in line with regulatory requirements and quality management procedures. Users will be informed of any changes that may affect device performance or instructions for use.
AI/ML Module within the AION Analytical Algorithm
This section provides specific information on the AI model embedded within the AION analytical algorithm. It explains its role within the device, its intended use, operational principles, and how it supports variant interpretation in a clinical context. This information complements the general description of the device and is provided to ensure transparency, clarity, and safe use of the AI-enabled components by qualified healthcare professionals.
Within the AION clinical workflow, the analytical algorithm integrates an AI/ML component together with established computational methods to support the classification of genetic variants. This component processes structured variant-level data enriched with curated reference information and produces probabilistic classifications into clinically relevant categories. The resulting outputs are combined with other analytical evidence within the AION system to generate variant-level classifications and a prioritised list of candidate disease-causing variants with their associated clinical diagnoses.
The AI model has been trained and validated on curated datasets designed to be representative of the intended clinical population, following established principles of data quality, fairness and bias mitigation. This ensures that outputs remain relevant across subgroups within the intended patient population.
The AI model has been validated on clinically relevant data and is designed to provide reliable decision-support outputs. As with all diagnostic support tools, results should be interpreted in the context of other clinical and laboratory information. The AI complements, but does not replace, the professional judgment of qualified healthcare professionals. All outputs are assistive in nature and are to be reviewed and confirmed by the responsible healthcare professional before being used in clinical decision-making.
The deployed AI model is a locked version (non-adaptive in the field), ensuring that no further learning or modification occurs post-release. It is maintained under controlled configuration management in accordance with relevant software lifecycle standards, with traceability to the training data, preprocessing pipelines, and source code version. All algorithmic outputs are presented within the system’s user interface (UI) alongside supporting evidence and explanatory metrics to aid interpretation.
Intended use of the AI/ML module within AION
All outputs are assistive in nature and require review and interpretation by qualified healthcare professionals. The AI module, referred to as Circe and implemented as an integrated subcomponent within the analytical algorithm of AION, serves to support variant classification by processing annotated germline variants and generating probabilistic pathogenicity assessments. It leverages multiple sources of genomic and clinical evidence to provide calibrated predictions that contribute to the overall variant classification framework. Outputs are assistive in nature, form part of the AION analytical algorithm workflow, and require review and interpretation by qualified healthcare professionals.
Indications for use of the AI/ML module within AION
The analytical algorithm component of AION is intended to identify diagnostic clinically relevant small variants (SNVs, indels), copy number variants and certain structural variants through automated variant interpretation (i.e. variant annotation, classification and prioritization), based on integrated molecular and phenotypic evidence. These outputs are intended to aid qualified healthcare professionals in diagnosing, screening or predicting the risk of genetic diseases in individuals or their descendants. The AI module within AION, is intended to assist in the classification of germline genetic variants identified through next generation sequencing (NGS) as disease-causing or benign in the context of Mendelian genetic disease testing.
This module is designed for use exclusively within the AION software environment and is not intended to be used as a standalone tool for direct medical decision-making.
The intended patient population includes individuals of all ages (prenatal and postnatal), sexes and ancestries, whose genomic data has been generated through validated NGS workflows for the purpose of genetic disease testing.
Intended users of the AI/ML module within AION
The intended users are licensed healthcare professionals (e.g., human genetics professionals, geneticists, laboratory professionals, variant scientists and healthcare practitioners with expertise in genetics). The software is not intended to be used by lay users or for self-testing.
No specialized training beyond the standard professional competence in genomic variant interpretation is required; however, users are expected to understand the principles of variant interpretation, and to have access to AION’s Instructions for Use (IFU). Users must also be aware that the analytical algorithm includes an AI/ML-based module for variant classification. The outputs are probabilistic in nature, reflect the operation of a trained statistical model, and must always be interpreted in context with other clinical and laboratory information
Operating principle of the AI/ML module within AION
The analytical algorithm component operates within the AION system to facilitate the interpretation of genetic variants in the context of genetic diseases. Its primary function is to leverage available case-level genetic and clinical data to detect clinically relevant genetic variants. This component processes case-level genetic data (i.e. VCF files) and when available, phenotypic features described using Human Phenotype Ontology (HPO) terms. It does not ingest raw specimens or raw sequencing reads.
The algorithm applies validated computational methods, combining curated genetic knowledge, established clinical guidelines, and statistical, algorithmic and AI-based approaches, to classify variants and prioritise candidate diagnoses. The outputs consist of variant classifications, phenotypic similarity measures, and prioritised lists of candidate diagnoses, which are presented for review by qualified healthcare professionals.
Operational environment of the AI/ML module within AION
The analytical algorithm component, including the Circe AI module, is fully embedded in the AION software ecosystem and cannot be deployed or operated as a standalone tool. Therefore, its intended operational environment is identical to that of AION. This includes use in professional healthcare or genetic testing laboratory environments, within the cloud-based AION infrastructure, accessed via supported web browsers and meeting the hardware/software requirements defined in the AION Instructions for Use (IFU).
AI Model Transparency, Human Oversight and Limitations
The AI/ML subsystem embedded in AION operates within clearly defined boundaries of transparency, autonomy, human oversight, trustworthiness, and usability. Requirements are established to ensure that users understand the model’s operational limits, that misuse is anticipated and mitigated, and that outputs are communicated in a clinically interpretable way.
The AI module is a locked model. It does not adapt or learn in the field and therefore maintains consistent behaviour across all use cases within its validated scope. Transparency is supported through the presentation of outputs that can be traced back to the underlying evidence and decision logic. In the UI, variant classifications are accompanied by uncertainty indicators, supporting evidence references, and explanatory metrics to facilitate interpretation. Explainability is addressed through both design-time documentation and user-facing features, allowing healthcare professionals to understand the basis of model outputs.
All outputs from the AI module are intended as decision-support and must be reviewed by qualified professionals. AION is not an autonomous diagnostic system, and its outputs are not to be used as standalone diagnostic conclusions. The system design ensures that human operators remain in the loop, particularly in cases where model confidence is low or where clinical contexts extend beyond validated scope.
To further ensure reliability, users are expected to confirm AI-suggested results against their own expertise and patient-specific information. Any unexpected or inconsistent outputs should be reported through the established feedback and customer support channels, allowing continuous monitoring of device performance and safeguarding the accuracy of the diagnostic process.
Predictability and fairness are addressed through systematic validation, ensuring that outputs behave consistently across a range of representative datasets. Known limitations and residual risks, including contexts with reduced model confidence or unsupported variant classes, are explicitly communicated through warnings in this IFU and within the AION interface. Safety and misuse prevention are managed through technical safeguards, user training, and clear communication of operational boundaries. Misuse scenarios, such as application outside the intended patient population or reliance on outputs without professional oversight, are anticipated and mitigated through the intended use, warnings, interface design, and system restrictions.
AION as a software system may undergo periodic updates in line with regulatory requirements and quality management procedures. Such updates may include improvements to the user interface, additional non-AI features, security enhancements, or maintenance of system components. Users will be informed of any updates that affect device performance or these instructions for use.
The AI model itself is deployed as a locked version, meaning it does not adapt or learn during use in the clinical environment. In the event that a new locked model version is released, this update will follow the controlled regulatory processes. Users will be notified of any new validated performance metrics, together with any changes or limitations relevant for clinical interpretation.
All significant AI/ML-related residual risks are included in the general Warnings and Limitations section of this IFU. These risks are communicated transparently to the user, ensuring that the AI component is understood as one part of the broader AION analytical algorithm, with performance metrics aligned with those of the AION system as a whole, covering sensitivity, specificity, accuracy and reproducibility as defined in the device’s performance evaluation.
Performance Characteristics of AION
AION’s tertiary analysis approach based on AI/machine learning effectively automates the process of variant interpretation of genetic tests for the diagnosis of rare genetic disorders. Machine learning (ML) and automated tools on genetic variant classification, prioritization, and interpretation in the context of diagnosing rare diseases have significantly enhanced the accuracy, efficiency, and reliability of genetic diagnostics by integrating deep phenotyping, genotype-phenotype knowledge, and advanced computational methods (AION’s scientific validity).
AION’s clinical evidence is gathered from published experience from routine diagnostic testing supported by other sources of clinical performance data, as synthetic datasets that simulates the complexities and variability of genomic data.
AION’s performance is evaluated based on the state of the art benchmarking approach for NGS-based genetic testing. It addresses both analytical and clinical AION’s performance specifications per genetic variant type (small variants and CNVs/SV) from a retrospective real patient data submitted by diagnostic laboratories across Europe, encompassing individuals who underwent clinical exome and genome sequencing for diagnostics of rare genetic disease, being supplemented by other sources of data as synthetic cohorts from a GIAB-derived benchmark “truth set”. AION’s analytical performance is determined by the analytical sensitivity, confidence intervals and precision (repeatability/reproducibility). AION’s clinical performance is determined by the diagnostic sensitivity, confidence intervals, PPV, rank (position of the causative variant in the prioritized variant list) and total number of unique variants (total number of variants in the prioritizer list). Analytical and clinical performance are presented separately for the two prioritization lists provided by AION: AION Clues (AC) and AION Smoking Guns (SG); CNVs/SVs are reported under AC.
A summary of AION’s analytical and clinical performance results is shown in the subsection below.
AION’s clinical performance based on published experience from routine diagnostic testing
A retrospective clinical cohort of 330 cases was assembled from real patient data submitted by diagnostic laboratories across Europe, encompassing individuals who underwent clinical exome and genome sequencing for diagnostics of rare genetic disease. These positive cases were carefully selected to evaluate AION because they reflect the diversity encountered in real-world diagnostic settings, including both technical complexities from varied laboratory workflows and clinical challenges presented by edge cases. Diagnostic variants were defined as variants considered clinically relevant and reported back to the clinician based on genetic, phenotypic, and segregation information from the patient.
Utilizing data from routine diagnostic testing offers significant value by providing insights from larger, heterogeneous and more complex populations. This cohort captures variations in wet lab protocols, sequencing approaches, secondary analysis workflows and the quality of clinical information available for analysis. Overall, the cohort included singletons and trios for small variants (trios exclusively in small variants), while CNVs/SVs were represented only as singletons. The cohort included 188 cases analyzed using the GRCh37 reference genome, including 135 cases with small variants and 53 cases with copy number variations (CNVs). The remaining 142 cases utilized the GRCh38 reference genome and included 106 cases with small variants and 36 cases with CNVs. For GRCh37, the cohort consisted of 40 trios (all with small variants) and 146 singletons (93 with small variants and 53 with CNVs). For GRCh38, the cohort included 79 trios (all with small variants) and 64 singletons (28 with small variants and 36 with CNVs)
To evaluate the influence of phenotypic data on variant interpretation, all cases were initially submitted with Human Phenotype Ontology (HPO) terms and subsequently re-analyzed without them. This diverse distribution of reference genomes, variant types and case structures ensures that the evaluation of AION’s performance accurately reflects the varied genomic configurations and clinical scenarios encountered in everyday diagnostic settings. This diversity is essential to identify less common, potentially serious device limitations and adverse events. By incorporating this comprehensive and varied data, our aim is to demonstrate AION’s capability to perform reliably across a wide range of clinical environments, ensuring robust and accurate variant interpretation in routine diagnostic workflows.
Table 3: Analytical and clinical performance results from the retrospective clinical cohort for SNVs (n=241) and CNVs/SVs (n=89). Analytical and Clinical performance is presented separately for the two prioritization lists provided by AION: AION Clues (AC) and AION Smoking Guns (SG). Results presented include a subset of the analytical performance results (analytical sensitivity, including confidence intervals), as well as clinical performance results (diagnostic sensitivity, including confidence intervals, positive predictive value (PPV), average variant rank and average number of unique variants). Analytical and clinical performance is presented separately for the two prioritization lists provided by AION: AION Clues (Table 3A) and AION Smoking Guns (Table 3B). CI: Confidence Interval, PPV: Positive Predictive Value.
Table 3A. Retrospective clinical cohort — AION Clues
|
Analytical performance results |
Clinical Performance results |
|||||||
|
Clinical cohort |
Dataset |
Analytical Sensitivity |
Analytical Sensitivity CI (95%) |
Diagnostic Sensitivity (Top‑3) |
Diagnostic Sensitivity CI (95%) |
PPV |
Rank |
Average # unique variants* |
|
GRCh37 with HPOs |
Small variants (n= 135) |
86.20% |
79.1%–91.6% |
80.10% |
72.29%–86.61% |
93.80% |
1.98 ± 0.03 |
9.51 ± 0.38 |
|
CNVs (n= 53) |
92.40% |
81.8%–97.9% |
92.4% |
74.66% - 94.52% |
94.60% |
1.4 ± 0.15 |
- |
|
|
GRCh37 without HPOs |
Small variants (n= 135) |
86.20% |
79.1%–91.6% |
51.90% |
43.01%–60.72% |
90.70% |
5.07 ± 0.53 |
10.3 ± 0.4 |
|
CNVs (n= 53) |
90.50% |
79.3%–96.8% |
90.5% |
79.3% - 96.8% |
94.50% |
1.8 ± 0.2 |
- |
|
|
GRCh38 with HPOs |
Small variants (n= 106) |
85.05% |
76.8%–91.2% |
70.10% |
60.48%–78.56% |
93.70% |
2.56 ± 0.3 |
9.3 ± 0.4 |
|
CNVs (n= 36) |
86.10% |
70.5%–95.3% |
80.56% |
63.98% - 91.81% |
94.2% |
1.6 ± 0.2 |
- |
|
*For CNVs/SVs, the “Average # unique variants” is not reported. Unlike small variants, CNV/SV analysis typically yields only a very limited number of candidates per case, making this metric not meaningful in the context of CNV prioritization. Therefore, results for CNVs/SVs are presented in terms of sensitivity, PPV and rank only.
Table 3B. Retrospective clinical cohort — AION Smoking Guns
|
Analytical performance results |
Clinical Performance results |
|||||||
|
Clinical cohort |
Dataset |
Analytical Sensitivity |
Analytical Sensitivity CI (95%) |
Diagnostic Sensitivity (Top‑3) |
Diagnostic Sensitivity CI (95%) |
PPV |
Rank |
Average # unique variants |
|
GRCh37 with HPOs |
Small variants (n= 135) |
75.5% |
72.3%–86.6% |
70.3% |
61.6% - 77.9% |
93.8% |
1.3 ± 0.06 |
2.56 ± 0.18 |
|
GRCh37 without HPOs |
Small variants (n= 135) |
3.05% |
0.84%–7.63% |
1.5% |
0.19% - 5.41% |
36.7% |
1 ± 0.00 |
0.16 ± 0.4 |
|
GRCh38 with HPOs |
Small variants (n= 106) |
70.09% |
60.4%–78.5% |
61.6% |
51.7% - 70.9% |
93% |
1 .1 ± 0.03 |
1.68 ± 0.1 |
Note: Smoking Guns (SG) results are reported for small variants only. CNVs/SVs are reported exclusively under AION Clues (AC), as SG is not available for CNVs/SVs in AION.
Performance in Small Variants
The small variant analysis cohorts provide real-world evidence of AION's use cases, reflecting its application in diverse clinical scenarios. For GRCh37, analytical sensitivity was 86.20%, while GRCh38 achieved a sensitivity of 85.05%. Diagnostic sensitivity was 80.10%80.10% for GRCh37 and 70.10%70.10% for GRCh38. These datasets include borderline and complex cases, offering valuable insights for performance optimization. Although the diagnostic sensitivity is slightly lower than that observed in synthetic datasets (see Summary of Performance Data from Other Sources available for comparative purposes), AION consistently prioritized disease-causing variants with an average rank of ~2 (GRCh37: 1.98 ± 0.03; GRCh38: 2.56 ± 0.3), demonstrating its reliability in handling diverse and challenging cases.
While HPO data do not directly affect AION’s analytical performance metrics, their inclusion significantly improves diagnostic sensitivity, confidence intervals, and variant ranking. Running AION without HPOs results in a substantial reduction in ranking performance, with the causative variant around the 5th position on average (5.07 ± 0.53) compared to ~2nd (1.98 ± 0.03) with HPOs. This underscores the importance of HPOs in enhancing AION's diagnostic capabilities. Consistently with this, SG shows strong performance when HPOs are provided but degrades without phenotype input; AC remains robust for sensitivity and mainly benefits from HPOs through improved ranking and review efficiency.
These findings align with observations from synthetic cohorts, although the effects of HPO inclusion are more pronounced in real-world cases than in GIAB-derived synthetic datasets. This indicates that HPOs are especially critical for improving AION's diagnostic performance in clinical settings. Consequently, we strongly recommend including HPOs in the analysis, as advised in the Instructions for Use, to maximize diagnostic accuracy.
The inclusion of HPOs had a significant impact on clinical performance metrics, notably diagnostic sensitivity, confidence intervals, and variant ranking. Without HPOs, AION's ranking performance decreased significantly, with the causative variant at ~5.07 ± 0.53 on the prioritized list compared to ~1.98 ± 0.03 with HPOs. This pattern was more prominent in the clinical cohort than in synthetic datasets, further emphasizing the relevance of clinical data in enhancing AION's diagnostic sensitivity. Despite the reduced performance in clinical cohorts compared to synthetic datasets, the observed trends are consistent, underscoring AION's adaptability to real-world variability and its potential to improve diagnostic outcomes in complex clinical environments.
Performance metrics differ between reference genomes, with GRCh37/hg19 outperforming GRCh38/hg38 in analytical and diagnostic sensitivity and confidence intervals. These differences may stem from the smaller GRCh38/hg38 cohort size, reduced annotation maturity, and variability in real-world cases. Clinical cohorts show lower sensitivity and wider confidence intervals compared to synthetic datasets, which rely on highly curated GIAB data with spiked-in variants and much larger sample sizes (>1,000 vs. 106/135). Despite these disparities, consistent trends across datasets underscore the need for optimized annotations and larger real-world datasets to further enhance AION’s diagnostic accuracy and clinical utility across reference genomes. Overall, these findings reaffirm the robustness of AION's clinical performance across reference genomes and emphasize the importance of selecting appropriate annotations to maintain diagnostic accuracy and consistency in clinical workflows.
Performance in CNVs/SVs
Copy Number Variants (CNVs) present unique challenges compared to small variants, primarily due to their reliance on upstream processes (e.g., sequencing and secondary analysis) to distinguish true disease-causing variants from false positives caused by sequencing artifacts. These challenges are further compounded by the relative rarity of CNVs in clinical practice, as they account for only about 10% of disease-causing variants in monogenic disorders. This scarcity limits the availability of robust benchmarking datasets for evaluating CNV detection and interpretation.
The analytical sensitivity for CNVs is 92.4% (95% CI: 81.8%–97.9%) for GRCh37 and 86.1% (95% CI: 70.5%–95.3%) for GRCh3892.4% (95% CI: 81.8%–97.9%) for GRCh37 and 86.1% (95% CI: 70.5%–95.3%) for GRCh38, comparable to that of small variants. However, the wider confidence intervals reflect the inherent variability and uncertainty in accurately interpreting larger structural changes. In the GRCh37 cohort for CNVs (n=16), AION demonstrated a diagnostic sensitivity of 92.4% (95% CI: 74.66%–94.52%)diagnostic sensitivity of 92.4% (95% CI: 74.66%–94.52%) and a precision (PPV) of 94.6%, highlighting its ability to accurately prioritize causative variants. The average rank of causative variants was 1.4 ± 0.151.4 ± 0.15, underscoring its reliable prioritization capabilities. In the GRCh38 cohort (n=36), analyzed using the current pipeline (v3.16.1.0), diagnostic sensitivity (Top-3) was 80.56% (95% CI: 63.98%–91.81%), PPV 94.2%, and average rank 1.6 ± 0.2In the GRCh38 cohort (n=36), analyzed using the current pipeline (v3.16.1.0), diagnostic sensitivity (Top-3) was 80.56% (95% CI: 63.98%–91.81%), PPV 94.2%, and average rank 1.6 ± 0.2, providing a benchmark for its performance in different reference genomes.
Establishing a comprehensive benchmarking dataset for CNVs remains particularly challenging. The rarity of these variants, coupled with variability in detection due to differing sequencing technologies, creates significant hurdles. Precisely identifying breakpoints is another complication, making validation efforts even more difficult. Despite these obstacles, ongoing improvements to CNV workflows and efforts to establish more reliable benchmarking standards are critical to enhancing AION’s performance in this area and bolstering its overall clinical utility. Although diagnostic sensitivity is largely comparable with and without HPOs in GRCh37 CNVs, including HPO terms improves ranking (e.g., ~1.4 with HPOs vs ~1.8 without), so we strongly recommend providing HPOs whenever available.Although diagnostic sensitivity is largely comparable with and without HPOs in GRCh37 CNVs, including HPO terms improves ranking (e.g., ~1.4 with HPOs vs ~1.8 without), so we strongly recommend providing HPOs whenever available.
Clinical performance for CNVs is strongly influenced by the inclusion of HPO data. Although the absence of HPO terms does not significantly affect diagnostic sensitivity, it has a notable impact on variant ranking, underscoring the importance of phenotypic data in CNV/SV analyses. While the optional nature of the HPO feature provides flexibility for users without phenotypic data, including HPO terms ensures more accurate and clinically relevant variant ranking. For optimal CNV/SV analysis, we strongly recommend incorporating HPO data (see the Limitations of Use and Contraindications section). Despite ranking impacts, AION maintains its ability to identify clinically significant variants, ensuring its diagnostic sensitivity aligns with its intended role as a clinical decision support tool.
Regarding the impact of the reference genome, an updated GRCh38 cohort (n=36) is now available and shows results analytically comparable within the same performance range and an updated GRCh38 cohort (n=36) is now available and shows results analytically comparable within the same performance range. Differences, particularly in confidence intervals, likely stem from the limited sample size in current CNV customer cohorts. Notably, PPV data remain consistent, although rank remains slightly tighter with HPOs across builds.
To address current limitations in datasets for CNV analysis, we are actively expanding our cohorts to include a greater number of samples, which will further enhance benchmarking reliability and performance evaluation.
Performance Conclusions
AION’s benchmarking results highlight its effectiveness in addressing diagnostic challenges, handling complex cases, and supporting clinical laboratories in managing their workflows. Its continuous validation process ensures alignment with current standards and regulatory requirements, contributing to its reliability as a tool for genetic diagnostics. These findings underscore AION’s potential to improve diagnostic workflows and deliver better outcomes for patients with rare genetic diseases.
Our results demonstrate the robust analytical and clinical performance of AION, highlighting its reliability, adaptability and impact in advancing genetic diagnostics. Analytical evaluations validate AION’s technical precision and consistency, while clinical assessments underscore its effectiveness in real-world diagnostic settings. The inclusion of phenotypic information through HPO terms further strengthens performance, particularly in CNV cases. In small variants, results are presented for both AION Clues (AC) and AION Smoking Guns (SG): AC remains robust for sensitivity and benefits from HPOs mainly through improved ranking, whereas SG shows strong performance when HPOs are provided and degrades without phenotype input.
The comparison between GRCh37 and GRCh38 reference genomes illustrates AION’s adaptability across different genomic assemblies, with advanced annotation resources in GRCh38 contributing to improved prioritization outcomes. With expanded real-world CNV cohorts (GRCh37 n=53; GRCh38 n=36) and updated analyses, AION demonstrates high sensitivity, stable PPV and favorable rank across builds;while the dependence on HPOs is less pronounced than in earlier assessments, including HPOs remains strongly recommended to optimize prioritization and streamline clinical review. Ongoing efforts to expand clinical datasets, particularly for GRCh38, will further enhance its validation and address existing gaps.
The results of these evaluations position AION as a state-of-the-art solution in genomic medicine. Its analytical and clinical performance showcases AION’s ability to deliver accurate, efficient and actionable insights for rare disease diagnostics. By bridging analytical precision with real-world applicability, AION sets a new standard for the integration of artificial intelligence in clinical genomics, reaffirming its value as a transformative tool for modern medicine.
Of note, limitations to these performance data include but are not limited to:
- Performance data for NGS tertiary analysis is limited by the lack of standardized benchmarking sets with validation cohorts that might not reflect real-world diversity (genetic backgrounds, etc.). Inconsistent data quality from different sequencing platforms and GDPR restrictions on data access further complicate the benchmarking process.
- Limitations regarding the availability of validation data sets for certain variant types (eg. CNVs/SV) shall be taken into consideration when evaluating these data as well as other limitations related to the state of the art benchmarking validation approach for NGS analysis (see limitations section for more details).
- AION’s clinical performance validation methodology is subjected to continuous improvement and to reference data set collection refinement by addition of novel gold set standards and/or real-world-data (CNV/SV variants limitation).
Results gathered in the tables above are representative of AION’s analytical and clinical performance and obtained from AION version v.3.16.1.0. Data updated on August 15th, 2025.
For more information see the white paper “Enhancing Rare Disease Diagnostics: Updated Performance Evaluation and Advancements of the AION AI-Driven Variant Interpretation Platform” available at the Nostos Genomic’s website Nostos Genomics - Latest News (nostos-genomics.com), under the section of Resources/Whitepapers
Summary of Performance data from other sources
Concerns over data privacy and security significantly limit access to large and diverse patient genetic and clinical datasets essential for robust validation. While real patient samples provide the most accurate assessments, these limitations prompted us to simulate genetic data for 4299 individuals with rare genetic diseases. We achieved this by introducing disease-causative variants into high-quality control reference genomes and linking this genetic data to its associated clinical phenotype. The variants and clinical data used in this process were meticulously identified and curated from reputable peer-reviewed publications and through collaborations with scientific research groups. This approach enabled the creation of an extensive and heterogeneous reference dataset, allowing for a comprehensive evaluation of AION’s variant interpretation capabilities at scale while effectively circumventing the privacy and security constraints associated with accessing actual patient genetic data. Results are presented separately for AION Clues (AC) and AION Smoking Guns (SG).
A comprehensive range of genetic scenarios was simulated to mirror the diverse conditions found in real-world clinical laboratories, ensuring AION’s reliability across various genomic configurations and data availability. This included both trios and singletons to evaluate performance in familial and individual cases, the use of GRCh37 and GRCh38 reference genomes for compatibility across different assemblies and simulations with and without clinical data encoded as Human Phenotype Ontology (HPO) terms to assess effectiveness under varying levels of phenotypic information.
ℹ️ It is important to note that these results from synthetic cohorts are not intended to serve as clinical evidence demonstrating the clinical performance of AION. Rather, they are included as supplementary data that can provide additional information on AION’s performance in synthetic cohorts, complementing the results obtained from real patient data.
Table 4: Analytical and clinical performance results from the synthetic validation cohort for Single Nucleotide Variants (SNVs) (n=42994299). Cases were analyzed as trios versus singletons to evaluate the impact of including parental genetic data. The analyses for the GRCh37 cohort were repeated with and without HPO terms to assess the effect of incorporating phenotype data. Additionally, the same cases were analyzed using reference genomes GRCh37 and GRCh38 to compare the impact of different genome assemblies on clinical performance. Results presented include a subset of the analytical performance results (analytical sensitivity, including confidence intervals), as well as clinical performance results (diagnostic sensitivity, including confidence intervals, positive predictive value (PPV), average variant rank and average number of unique variants). Analytical and clinical performance is presented separately for the two prioritization lists provided by AION: AION Clues (Table 4A) and AION Smoking Guns (Table 4B). CI: Confidence Interval, PPV: Positive Predictive Value.
Table 4A. Validation cohort — AION Clues
|
Analytical performance results |
Clinical Performance results |
|||||||
|
Validation cohort |
Dataset (n=4299) |
Analytical Sensitivity |
Analytical Sensitivity CI (95%) |
Diagnostic Sensitivity (Top‑3) |
Diagnostic Sensitivity CI (95%) |
PPV |
Rank |
Average # unique variants |
|
GRCh37 with HPOs |
Trios |
95.79% |
95.42%–96.60% |
95.70% |
95.15%–96.37% |
94.79% |
1.08 ± 0.005 |
2.02 ± 0.005 |
|
Singletons |
91.25% |
90.30%–92.08% |
91.25% |
90.30%–92.08% |
94.50% |
1.02 ± 0.005 |
1.98 ± 0.005 |
|
|
GRCh37 without HPOs |
Trios |
95.90% |
95.90%–96.50% |
95.90% |
95.20%–96.50% |
94.80% |
1.63 ± 0.01 |
3.8 ± 0.02 |
|
Singletons |
91.42% |
90.50%–92.20% |
91.40% |
90.50%–92.20% |
94.50% |
1.51 ± 0.01 |
3.8 ± 0.03 |
|
|
GRCh38 with HPOs |
Trios |
96.05% |
95.42% - 96.6% |
96.05% |
95.4% - 96.6% |
94.8% |
1.07 ± 0.002 |
4.04 ± 0.03 |
|
Singletons |
91.56% |
90.68% - 92.3% |
91.56% |
90.68% - 92.3% |
94.6% |
1.02 ± 0.002 |
3.9 ± 0.02 |
|
Table 4B. Validation cohort — AION Smoking Guns
|
Analytical performance results |
Clinical Performance results |
|||||||
|
Validation cohort |
Dataset (n=4299) |
Analytical Sensitivity |
Analytical Sensitivity CI (95%) |
Diagnostic Sensitivity (Top‑3) |
Diagnostic Sensitivity CI (95%) |
PPV |
Rank |
Average # unique variants |
|
GRCh37 with HPOs |
Trios |
90.84% |
90.18%–91.90% |
90.80% |
89.90%–91.60% |
94.50% |
1.02 ± 0.001 |
1.15 ± 0.02 |
|
Singletons |
87.00% |
85.90%–88.00% |
87.00% |
85.90%–88.00% |
94.30% |
1.01 ± 0.001 |
1.11 ± 0.02 |
|
|
GRCh37 without HPOs |
Trios |
1.35% |
1.03%–1.74% |
1.35% |
1.03%–1.74% |
20.4% |
1.00 ± 0.00 |
0.01 ± 0.00 |
|
Singletons |
1.35% |
1.03%–1.74% |
1.35% |
1.03%–1.74% |
20.4% |
1.00 ± 0.00 |
0.01 ± 0.00 |
|
|
GRCh38 with HPOs |
Trios |
91.07% |
90.18% - 91.9% |
91.07% |
90.68% - 92.3% |
94.5% |
1.07 ± 0.002 |
1.15 ± 0.003 |
|
Singletons |
87.4% |
86.19% - 88.2% |
87.23% |
86.19% - 88.2% |
94.3% |
1.01 ± 0.003 |
1.13 ± 0.008 |
|
The trio analysis demonstrates higher analytical sensitivity and improved confidence intervals for sensitivity, indicating reduced bias in the trio-based approach. Regarding clinical performance, results for small variants reveal enhanced diagnostic sensitivity with the trio approach, reflected in less biased sensitivity confidence intervals. There are no significant differences in Positive Predictive Value (PPV) or variant ranking. Importantly, incorporating parental genetic background (trios) significantly impacts the total number of identified variants and associated performance metrics in variant classification and prioritization. Clinical performance data align with the analytical performance trends, particularly in sensitivity and confidence intervals. However, variant rankings remain consistent, suggesting that while variant discovery and performance metrics improve with trios, the prioritization process itself remains stable. These conclusions apply to both AC and SG
Clinical information input (e.g., HPO terms) does not significantly affect AION’s analytical specifications. For clinical performance, results from synthetic cohorts show that HPO data have minimal impact on diagnostic sensitivity in the trio approach, as parental information provides sufficient clinical context. Conversely, in the singleton approach, where only the proband file is analyzed, diagnostic sensitivity significantly decreases in the absence of HPO terms. Furthermore, in singletons without HPO data, variant ranking drops, with the causative variant averaging the third position in the prioritized list, compared to the first position when HPO terms are included. Therefore, optimal variant prioritization (ranking) requires patient clinical data (HPO terms) as input. In SG, the role of HPOs is critical: these evaluations are designed as a strict prioritization challenge in which phenotypic data are required for meaningful results. Without HPO input, performance drops to non-actionable levels, while with HPOs both GRCh37 and GRCh38 demonstrate strong and consistent performance (see Table 4B). This dependency is explicitly acknowledged as a limitation in the Instructions for Use, emphasizing the importance of providing phenotype data whenever available.
AION’s analytical performance is not significantly affected by the choice of reference genome, regardless of the genetic analysis approach (singleton vs. trios). The observed trend of enhanced analytical performance in trios compared to singletons ((e.g., for AC with HPOs: GRCh37 trios 95.79% vs. singletons 91.25%; GRCh38 trios 96.05% vs. singletons 91.56%) remains consistent across reference genomes. A similar trio-over-singleton pattern is observed for SG with HPOs (GRCh37 90.84% vs. 87.00%; GRCh38 90.77% vs. 87.54%)) remains consistent across reference genomes. Clinical performance evaluation indicates some differences between reference genomes; however, these differences are within acceptable performance criteria and align with expected outcomes. These findings confirm the robustness of AION’s clinical performance across reference genomes, emphasizing the importance of selecting appropriate annotations to ensure diagnostic accuracy and consistency in clinical workflows
Intended Environment
The typical use environment is an office or genetic testing laboratory.
AION runs on cloud computing.
Browser specifications to run AION are as follows. Minimum hardware requirements to run app UI, the minimal requirements would be:
-
A device with 2GB of RAM or more
-
A recent version of a web browser (such as Google Chrome, Firefox, Safari, or Microsoft Edge)
-
A CPU with 2 cores or more
-
A resolution of 1024x768 or higher
Limitations of use and contraindications
AION’s indications of use relate to mendelian genetic diseases, consequently interpretation of variants that may not follow traditional mendelian patterns (such as somatic variants implicated in cancer or pharmacogenetics, PGx) is currently excluded from the indications of use (“limitations of use or contraindications”). Thus:
- AION is not intended for the analysis of somatic variants implicated in cancer.
- AION is not intended for gene-drug association analysis or drug dosing recommendations based on pharmacogenetic variant analysis (PGx). It is also not intended for biomarker analysis in combination with therapeutic drugs (companion diagnostics, CDx).
- AION is not intended for the interpretation of genetic variation associated with trisomy 21, diagnosing phenylketonuria and determining HLA tissue types DR, A and B.
AION mitigates the risk of use for the diagnosis of the aforementioned conditions out-of-device's intended use through different approaches, including the design of the user interface for case submission, as well as quality controls within the genetic analysis pipeline.
- Somatic variants implicated in cancer. The analysis of somatic variants in a tumor would typically require the submission of a tumor sample and a germline sample for comparison. The submission of this type of analysis is not supported by the device, which only allows for the uploading of VCF files including two formats: 1) singleton (only proband) or 2) trio (proband, mother and father). Furthermore, variants with a variant allele frequency deviating from the expectation for germline variants (i.e. somatic variants with a VAF < 20%) are flagged in our quality control module of the analysis and are excluded from the prioritized results.
Additional control mitigating actions to prevent the risk of AION reporting variants out of its intended use, include a meticulous manual curation of AION’s datasets (gene-disease dictionaries), in order to ensure that only clinically relevant Mendelian diseases are retained and variants included on AION’s intended use reported. This process effectively excludes the majority of somatic cancer-related diseases (exclusion criteria):
- Late-onset somatic mutations
- Diseases requiring additional disease processes (e.g. clonal expansion of mutated hematopoietic stem cells) to manifest.
- Disease heavily influenced by environmental factors.
- Complex multigenic diseases where no single gene mutation can definitively be linked to the disease phenotype.
- Pharmacogenetic variant analysis and companion Dx. AION user interface does not support uploading of information related to patient’s drug prescription and treatments, which are needed for pharmacogenetics and companion diagnostics analysis. In addition, the platform is not intended to provide or analyze pharmacogenetic information:
- AION does not include specific data related to pharmacogenes or gene-drug interactions.
- AION does not rely on any dedicated PGx database (such as PharmGKB, CPIC, etc.), but on data from OMIM (Online Mendelian Inheritance in Man), which is not comprehensive for PGx purposes as it does not explicitly tag pharmacogenetic relationships. Nevertheless, AION datasets have been manually curated to exclude diseases potentially associated with susceptibility factors and connected to pharmacogenetic data within OMIM.
- AION currently does not contain genes with clear ties to pharmacogenetics in the context of drug metabolism. For example, genes like CYP2D6 and CYP2C9—key players in pharmacogenetic analysis—have been removed to ensure compliance with AION's exclusion policy.
- Genetic variation associated with trisomy 21.The diagnosis of trisomy 21 is typically carried out through other methods such as karyotypes where an aneuploidy can be directly visualized or by microarray to observe the increase of signal indicating aneuploidy. The output files from these methods and the type of genetic variation detected are not compatible with AION’s platform, which only allows for uploading VCF files containing SNVs, indels, CNVs and SVs in one of the following two formats: 1) singleton (only proband) or 2) trio (proband, mother and father). Consequently, it will be rejected during analysis, indicating to the user that an error has occurred due to file incompatibility.
Of note, although AION’s analysis results could potentially include variants associated with somatic mutations, variants with companion diagnostic indications, or other variants listed as limitations/contraindications the mechanisms reported herein efficiently mitigate the reporting of these variants and ensure that only variants included on AION’s intended use are reported.
Nevertheless, AION is contraindicated for somatic variants, T21 and PGx, and it is responsibility of the healthcare professional as intended user of AION to acknowledge this potential foreseeable device’s misused.
Predictions generated by the software are probabilistic outputs and must not be interpreted as definitive classifications of variant pathogenicity. In particular, predictions for loss-of-function variants reflect the distributional properties of the available data and should be considered as inputs into the broader decision-support workflow. Final interpretation of variant significance requires integration with downstream filtering, annotation, and expert review steps.
Additional limitations of use of AION are related to:
- Device’s analytical performance: AION supports gene panel data prioritisation as long as there is data within the supported regions. The supported regions for prioritisation are:
- Coding regions
- ±50 bp around coding regions
- Known variants from ClinVar outside of these regions are also included in the analysis
- Device’s performance testing limitations (benchmarking): AION’s benchmarking-based performance testing includes limitations regarding to the control reference datasets, such as:
- The control dataset shares a uniform genetic background, so the device’s performance across different ethnicities has not yet been evaluated.
- The control dataset does not include variants located on chromosome Y (chrY) or mitochondrial DNA (chrMT).
- The control dataset is limited to unaffected singletons and parent-child scenarios..
- Control genomes from GIAB are of exceptionally high quality and lack the artifacts that may be present in actual customer cases, resulting in a potential risk of overfitting throughout device’s performance testing.
Of note, to avoid these limitations additional performance datasets from real world data is used for AION’s performance evaluation.
Additional limitations to the state-of-art benchmarking approach for NGS tertiary analysis performance evaluation are indicated at the end of the Performance characteristics section.
- Effect of HPO terms on variant prioritization: The inclusion of HPO terms is crucial for optimizing variant prioritization in genetic analysis. This is particularly relevant for both small variants (singleton cases) and CNVs/SVs. For small variants, the addition of HPO terms enhances the performance of variant ranking, improving the algorithm’s ability to identify clinically relevant findings. Although the absence of HPO terms does not compromise the diagnostic sensitivity of the software, it impacts its ability to effectively prioritize variants, potentially delaying or complicating clinical interpretation.
In the case of CNVs, the importance of HPO data is even greater due to the inherent complexity of analyzing these types of variants. Without phenotypic information, the software’s capability to prioritize relevant CNVs is diminished, increasing the risk of overlooking significant findings or misinterpreting results. To mitigate this, it is strongly recommended to include HPO terms for CNV/SV analysis. The absence of phenotypic data is a limitation and a potential risk that may impact the analysis’s clinical utility. Including HPO terms is essential for achieving accurate and clinically acceptable analysis results.
Similarly, the AION Smoking Guns prioritization strategy is highly dependent on HPO data. These evaluations are designed as a strict prioritization challenge in which phenotypic context is required for optimal performance. Without HPO terms, the algorithm defaults to reporting only a minimal set of variants that might be considered clinically relevant in the absence of phenotype data. This leads to a marked degradation in ranking, with even “crystal-clear” pathogenic variants no longer consistently appearing in the relevant range. With HPO terms provided, however, Smoking Guns demonstrates robust and clinically meaningful performance.
- Input VCF files quality. The quality of the VCF files, influenced by the secondary analysis performed by users, is crucial for optimal results, please see AION requirements for more information on VCF input data and recommendations for secondary analysis best practices.
- Sequencing technologies. AION’s quality control module includes tools to detect potential artifacts associated with specific sequencing technologies. We have also implemented a control list of artifacts (including information from over 200 VCF files and from scientific literature, Maffucci et al, 2018), which filters out variants commonly associated with sequencing errors across various platforms.In addition in the IVDB (Internal Variant Database) feature the software compute frequencies internal to each lab, and they could add specific filters, according to its potential sequencing artifacts.
- Short-read platforms
- AION has been designed and thoroughly validated with Next Generation Sequencing data from short-read platforms, mainly from Illumina technology.
- Data from IonTorrent platforms and its evolutions are supported, but have produced many artifacts. Before using it, we recommend to AION's users that the VCF data has been filtered for common artifacts from their setup.
- Long-read platforms.
Data from long read technologies has not been thoroughly tested. If you need to run samples with this type of data, we recommend you get in touch so we can quickly troubleshoot any potential issues and make sure the results have high quality.
- AION is a AI/ML-based tertiary analysis software. ML-based automated variant interpretation faces challenges such as incomplete analysis due to specialized algorithms, poor input data quality, and performance variability across diverse populations due to biased variant databases. Furthermore, though the algorithm is designed to classify genetic variants with high accuracy, it is not infallible. Incorrect variant classification predictions by ML-based algorithms might lead to the exclusion of clinically relevant variants from analysis and results (false negatives or false positives).
As a clinical decision support software, we recommend the healthcare professional to use the algorithm's results as a supportive tool rather than the sole basis for clinical decisions, and recommend that they conduct additional validation or consult with clinical experts when interpreting results to ensure accurate diagnosis and patient care.
Additional precautions or warnings are disclosed at AION’s Safety information section within this Instructions for Use.
Training for users
Users can request or schedule training sessions during the demo and onboarding trial period. These sessions are designed to cover the initial setup of AION, the key functionalities of AION and learn how to use them effectively, and common troubleshooting and support strategies.
To schedule a session, please contact us at:
- Website: nostos-genomics.com
- Email: support@nostos-genomics.com
However, these Instructions for Use provide all the essential information needed for the safe and effective operation of AION. These instructions also include visual support with clickable flows to enhance user guidance.
Additionally, in the “Example Use Cases” section, we provide practical examples illustrating how AION can assist in identifying causative variants in patients. These cases include both clinical information as well as VCF files for users' training.
For more information or additional assistance, please feel free to contact our support team.
Safety Information
Please see AION-IFU section Safety Information for product safety information in English and applicable EU members' languages.
The Summary of Safety and Performance is available here.